Pressure areas are the most fearsome issue confronting rehab and seating occupational therapists. “I will do anything to avoid it,” occupational therapist Sybbi Georgiou, from Megalong Positioning Service told F2L. “Even if a person does not have a pressure injury there is a lot of importance placed around prevention.
“Once a person has a pressure injury they always have it. As the patient slowly deteriorates, whatever their condition, the pressure area can quickly become a stage III pressure ulcer that can develop into more serious medical conditions. What happens is that the ulcer can heal over but because it is the weakest spot it can break open again.”
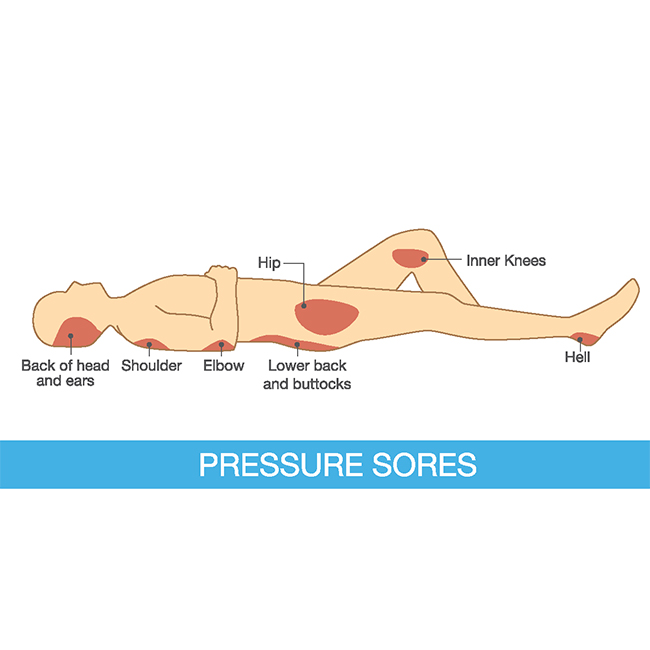
Prevention is critical in people who don’t move or can barely move, for example if a person is in a wheelchair, is older, has always had a disability or sleeps for long periods and have bony protuberances close to the skin that make them more susceptible, she said. “Pressure ulcers can be prevented by using support devices including cushions, mattresses and overlays.”
One of the major challenges facing OTs in pressure care management is knowing their role in the multidisciplinary team – how to work with other health care professionals such as nurses and physiotherapists.What aspects of management and prevention does each profession take on, and how is this communicated?, occupational therapist Emelia Young, from disability services group Yooralla, told F2L.
Another challenge is implementing pressure injury prevention guidelines in the community setting, where there is no consistent follow through and limited training for health care providers and carers. “When there is an assumption of knowledge, combined with insufficient information available there is an increased risk of pressure injury development,” Young said.
For wheelchair users in the community intervention needs to be functional and without this consideration during prescription equipment often goes unused and pressure issues develop.
“I see it that a partnership or interdisciplinary team approach to pressure care equipment prescription and prevention is vital, to ensure it is the right fit for all aspects of the person’s life,” she said. “Obviously when significant pressure care issues are present (ie. Stage 4 IT wound) you have to manage the acute wound. However, when we look at a preventative approach the above is possible.
“Unfortunately we can’t rely purely on pressure care equipment, there is a human factor to reducing pressure injury that must be considered and unfortunately this is more difficult to implement due to funding restrictions and models of care.”
When it comes to useful prevention strategies and equipment, it is the simple things that can often be extremely beneficial such as the use of sheepskin and bed mechanics and a 24-hour positioning clock: “What is the person doing, how long are they in the chair versus bed versus commode?”
One of the big challenges for OT is while there is lot of product on the market, and it would be unusual not to find a product that suits, it often comes down to cost, according to OT Rebekah Cranmer. “Also there are still people with pressure injuries with problems which are not necessarily a result of the equipment they are using but the nature of their movement disability,” Cranmer said.
“We know that with a pressure injury that is severe the best treatment is lying down and having complete bed rest to stop the progression of pressure injury as quickly as possible. With long standing pressure injuries the recommendation usually means six weeks in bed.”
The growing prevalence of pressure ulcers is expected to drive demand for pressure relief devices such as therapeutic support surfaces, mattresses and cushions. The rising prevalence of obesity is also predicted to fuel growth with obese patients said to be at increased risk of developing pressure ulcers as they are required to stay in hospital for longer periods and have slower wound-healing times, according to a US report on the medical devices industry.
In Europe, significant growth is also coming from the rising number of patients diagnosed with pressure ulcers coupled with a growing geriatric population. The availability of advanced pressure devices such as air therapy mattresses has contributed to growth too. However skilled personnel and the high cost of these devices have restricted demand to some extent. Low tech devices are said to be benefiting from cost effectiveness and ease of use and are sub-segmented into foam, gel and air-filled mattresses.